Skip to site content
It is no secret that as we age our bodies undergo changes that can increase the risk of developing health related issues. One of these health concerns is the susceptibility of forming a chronic wound. Chronic wounds are wounds that fail to heal within three months or more. They can be painful, debilitating, and can significantly impact the quality of life of the person suffering with a non-healing wound. Which is why this May, the Center for Wound Healing and Hyperbarics is acknowledging Older Americans Awareness month and offering nine tips to prevent and manage chronic wounds.
Senior Americans are at an increased risk of a hard to heal wound forming. In fact, seniors make up 85% of all chronic wound cases, and it is estimated that 8.2 million seniors above the age of 65 will develop a wound. Even though wounds can be the result of many different things as the skin becomes thinner with age, there are several factors that can increase the risk of developing chronic wounds in seniors, including diabetes, heart disease, limited mobility, dietary habits, and even medications.
The positive side is that chronic wounds are not developed overnight, and with the appropriate prevention and management techniques, they do not have to become life threatening. The prevention and management of chronic wounds in seniors involve a comprehensive approach that includes proper wound care, healthy lifestyle habits, and management of underlying health conditions. Here are some tips for preventing and managing chronic wounds in seniors:
Chronic wounds can significantly impact a senior's quality of life, and impact the majority of the American elderly, but with proper prevention and management, they can be avoided and treated when needed. Seniors can reduce their risk of developing chronic wounds by following a healthy lifestyle, managing chronic health conditions, and seeking timely medical care for wounds that do not heal. By following these tips, seniors can maintain their independence, mobility, and quality of life. If you or someone you love has a non-healing wound, give us a call at 580.531.6441 or visit SWMConline.com/wound-care for more information and assistance.
March is National Nutrition Month, a time to highlight the critical role nutrition plays in overall health. At the Center for Wound Healing and Hyperbarics at Southwestern Medical Center, we see firsthand how poor nutrition can contribute to non-healing wounds, particularly in patients with diabetes, cardiovascular disease, and other chronic conditions. These wounds, often located on the lower limbs or feet, can stall in the healing process for over 30 days, significantly impacting quality of life. At this stage, specialized wound care is essential to prevent infection and reduce the risk of amputation.
In the U.S., a limb is amputated due to diabetes every 3 minutes and 30 second, with up to 80% of non-traumatic lower limb amputations linked to diabetes complications. Because nutrition plays a key role in diabetes and other chronic conditions, a comprehensive wound care treatment plan must include a thorough assessment of the patient’s dietary intake to support healing and long-term health.
“At the for Wound Healing and Hyperbarics, we discuss dietary habits at every visit and encourage patients to think of the food they eat as medicine for their body,” said Jennifer James, MD, Medical Director. “Good nutritional habits can go a long way in terms of faster wound healing. Eating right can also help prevent the development of chronic wounds in the future.”
According to the Academy of Nutrition and Dietetics nutritional needs change as we age, and our diets occasionally need to be adjusted. Many wound care patients are seniors with underlying health issues and nutritional intake is a key component of the healing process. Here are six tips to help make positive dietary changes:
Multivitamins and mineral supplements are sometimes recommended for patients who do not consume an optimal diet or have medical conditions that impact nutritional intake. A supplement can help fill in the gaps. Discuss supplementation with your physician before starting one.
If you feel that your nutritional challenges are complicated and additional support is needed, a Registered Dietitian (RD) can help you learn about nutrition and create a customized eating plan. Medical nutrition therapy with an RD is covered by most insurance plans as well as Medicare Part B. For more information or if you have a non-healing wound, give us a call at 580-531-6441 or click here.
The Center for Wound Healing and Hyperbarics at Southwestern Medical Center is recognizing American Heart Month by offering information and tips to educate patients about heart health and non-healing wounds. Heart disease is the leading cause of death in Americans, and each year nearly 700,000 Americans are diagnosed with heart disease, which causes about 1 in 5 U.S. deaths, according to the Centers for Disease Control (CDC). Related complications like vascular insufficiency or peripheral arterial disease (PAD) can result in the development of non-healing wounds putting patients at risk of infection, sepsis, or lower limb amputation.
Due to an aging population as well as an increase in heart disease, diabetes and obesity, the need for specialized wound care continues to grow. Currently, there are up to 8 million Americans suffering from hard to heal wounds. Many patients postpone treatment with hope that their wound will heal on its own, only to seek treatment after it has become severely infected.
“It is not uncommon for cardiology patients to develop painful, non-healing wounds stemming from poor circulation to the lower extremities,” said Dr. Jennifer James, Medical Director, Center for Wound Healing and Hyperbarics. “If left untreated, this can progress to a life-threatening condition. It’s important for anyone with a non-healing wound to talk to their doctor as early as possible and get an evaluation in order to avoid sepsis or amputation.”
Common Wound Types in Patients with Cardiovascular Disease
Without proper blood flow from the heart, chronic wounds can develop and not only fail to heal, but they can grow in size and become infected. Here are the three most common non-healing wounds for patients with heart disease:
Tips for Better Heart Health
If you have heart disease or are in treatment for a non-healing wound, it’s important to pay attention to your cardiovascular health. A healthy heart stimulates the circulation of oxygen and nutrient-rich blood throughout the body, skin, and tissues and stimulates the body’s healing process. Here are six tips:
At the Center for Wound Healing and Hyperbarics, we’re using advanced wound care modalities and hyperbaric oxygen therapy to treat non-healing wounds caused by cardiovascular disease complications including venous and arterial ulcers. Chronic wounds can be diagnosed, effectively managed and ultimately healed, oftentimes within eight weeks. If you or someone you love has a non-healing wound, give us a call at 580-531-6441 or click here for more information and assistance.
Chronic Venous Insufficiency (CVI) occurs when the veins in the legs struggle to properly return blood to the heart, often due to malfunctioning valves. This condition affects millions, contributing to complications like varicose veins and venous leg ulcers (VLUs). Varicose veins impact up to 25 million Americans annually, while over 600,000 individuals develop venous leg ulcers each year, making VLUs one of the most common—and challenging—manifestations of CVI.
A hallmark symptom of CVI, and a precursor to venous ulcers, is lower leg edema. The swelling often feels like an inflated balloon, stretching the skin and causing discomfort. As blood pools in the veins, the skin may also darken or harden over time. Common symptoms include:
"Accounting for 90% of all lower limb ulcers, venous leg ulcers can persist from weeks to years, often leading to complications such as osteomyelitis, cellulitis, and, in rare cases, malignant changes," explains wound care specialist Catherine Yore, PA. "These ulcers significantly impact a patient’s quality of life and increase the risk of morbidity and mortality. That’s why preventive measures and treatments, like compression therapy, are essential for managing CVI and venous ulcers."
Compression therapy is widely regarded as the gold standard in managing VLUs, promoting better blood flow and reducing swelling.
Given their high recurrence rate, patients with CVI—or those who have already developed a venous ulcer—are encouraged to adopt lifestyle changes to support healing and reduce the risk of further ulceration. Key recommendations include:
By committing to these practices, patients can take proactive steps toward improving their overall vascular health and preventing complications.
CVI is a manageable condition when addressed early, but ongoing care and lifestyle adjustments are critical for long-term success. If you or someone you know is experiencing symptoms of CVI, consult with a healthcare provider for tailored guidance and support.
At the Center for Wound Healing and Hyperbarics at Southwestern, we’re using advanced wound care modalities and hyperbaric oxygen therapy to treat non-healing wounds caused by venous insufficiency. Stalled wounds can be diagnosed, effectively managed and healed, oftentimes within eight weeks. If you or someone you love has a non-healing wound, give us a call at 580-531-6441 or click here for more information.
It's important to understand the impact holiday traditions can have on the body’s health and healing process. For instance, walking around the neighborhood caroling in below freezing temperatures, while drinking hot chocolate that’s more marshmallow than cocoa, could cause any progress in healing to stall from added stress and inflammation. However, a wound doesn’t need to steal the holiday cheer, or cause any bah-humbug moments, so here are five helpful tips to make sure all of those living with a non-healing wound have a healthy and cheerful holiday season:
Bonus Tip for Wound Care Patients: Be sure to keep your regularly scheduled appointments and follow dietary recommendations. It’s very important to continue treatment throughout the holiday season and have an open line of communication with your care team.
If you have questions or would like more information on diabetes and wound care, click here or contact the Center for Wound Healing and Hyperbarics at Southwestern Medical Center at 580-531-6441.
November is Diabetes Awareness Month, a time to bring attention to this fast-growing, life-threatening epidemic. Currently more than 38 million Americans have diabetes and this number is expected to increase to 54.9 million by 2030. An increase in Diabetes has been attributed to a rise in obesity rates and an aging population, but new research shows that younger people are being diagnosed with the disease. From 2001 to 2017, the number of people under age 20 living with diabetes increased by 45 percent, and the number living with type 2 diabetes grew by 95 percent. This troubling development is expected to further challenge the healthcare system in the coming decades.
As the number of newly diagnosed diabetics increases, the incidence of complications including diabetic foot ulcers and related amputations is also on the rise. The COVID-19 pandemic has impacted young people with diabetes due to sudden and extended social isolation, sedentary lifestyles, treatment delays, and a general lack of consistency in disease management. Recent data reveals a 29 percent increase in diabetes related deaths for younger people last year.
Diabetic Foot Ulcers: The Most Common Cause of Hospitalization Among Diabetics
The most common cause of hospitalization among diabetics is a diabetic foot ulcer (DFU), or an open sore on the lower limb that becomes infected. DFUs typically develop on weight-bearing areas of the foot, most commonly the bottom of the big toe, the ball of the foot or the heel. Approximately 19 to 34 percent of individuals with diabetes will be diagnosed with a DFU at some point in their lives, and one in five of these patients will undergo a lower limb amputation. In fact, every 20 seconds a diabetes-related amputation is performed. The five-year mortality rate is upwards of 74 percent for patients with lower extremity amputation - higher than those for several types of cancer including prostate, breast, and colon combined.
Why are diabetics more vulnerable to foot ulcers and chronic wounds?
Uncontrolled blood sugar levels deprive the blood vessels of much-needed oxygen and nutrients, which are necessary for healing. To complicate things further, many individuals with diabetes have a loss of sensation in the lower limbs stemming from diabetic neuropathy. They may be unaware that a wound exists. On occasion, a trip to the ER for a high fever results in the discovery of a non-healing wound that has become infected. Many individuals with diabetes also have peripheral artery disease causing compromised blood flow to the feet, exacerbating the severity of the wound.
What do people with diabetes need to know?
A simple cut or scrape can quickly develop into a severely infected wound that does not heal and may be life-threatening. If a diabetic ulcer is suspected or discovered, a physician should be contacted immediately for an evaluation and possible referral to a wound care specialist. The general rule of thumb for most people is if a wound hasn’t healed on its own within 30 days, it should be evaluated. But if a patient has diabetes, early intervention is critical. With proper treatment, complications can be avoided.
“It’s important for people to know that a chronic wound in a diabetic patient can become infected quite quickly because of poor circulation,” said Jennifer James, MD at medical director at the Center for Wound Healing and Hyperbarics at Southwestern Medical Center. “If a patient gets evaluated early on, commits to treatment and is compliant with instructions, it will help prevent amputation.”
Wound care tips for individuals with diabetes:
Chronic wounds can be diagnosed, effectively managed and ultimately healed, oftentimes within eight weeks. Contact the Center for Wound Healing and Hyperbarics at 580-531-6441 for more information or click here.
August, the last official month of summer, is the perfect time for final pool parties and beach days. However, it can also bring heat waves and the consequences of a summer spent barefoot and in the water. For the 38.4 million Americans living with diabetes, this final month of summer can be particularly challenging for the body, which has already endured too much sun and not enough hydration.
The heat makes the beach, poolside, or patio ideal spots to celebrate warm summer nights. However, it's essential to aim for mornings without new wounds—or headaches. “Jennifer James, MD, medical director of the Center for Wound Healing and Hyperbarics at Southwestern Medical Center explains, "For those with diabetes, especially those experiencing neuropathy, regular foot checks are essential after a long summer night out.”
As you enjoy the End of Summer Bashes, remember to practice some CCR when you get home. No, we don’t mean whipping out the turntable, but checking for Cracks, Cuts, and Red-areas:
If any of these signs are present, the risk of developing a diabetic foot ulcer is higher and should be monitored closely. If healing does not begin within the first two days, especially if the skin has broken, contact a doctor immediately for further investigation.
While checking your feet, remember the acronym SUMMER:
At the Center for Wound Healing and Hyperbarics, we want to remind everyone at risk of developing non-healing wounds to be mindful of hot walking surfaces, even after sunset. When in doubt, don’t kick off your dancing shoes, even if the moon is high in the sky. If you do need to remove your shoes, check the walking surface with the back of your hand; if it's warm to the touch, it’s too warm for the bottom of your feet.
To help you know when a walking surface is too hot, follow this easy temperature guide for a Woundless Summer:

At the Center for Wound Healing and Hyperbarics, we want all our patients and those living with diabetes to enjoy this final month of summer safely. If you or someone you know develops a wound, please contact us at 580.531.6441 to get in touch with our care team.
Road trips and camping are a summer fan favorite to get to far out destinations, and they are an excellent time to practice singing skills, sit for long periods of time, load up on junk food, and enjoy the great outdoors. However, for those that are at risk of developing a pressure injury, road trips and outdoor activities can do extensive harm to the body.
Pressure injuries, also known as pressure ulcers or bedsores, are localized injuries to the skin and underlying tissues. They typically occur over bony prominences and are caused by prolonged pressure, friction, and shear forces. Pressure Injuries affect up to 3 million Americans each year, and can develop in less than 3 hours for those with underlying conditions like heart disease, immobility, and obesity.
“If you are at risk of a pressure injury, you need to be consistent about repositioning pressure and doing skin checks, but summer is particularly important,” said Jennifer James, MD, medical director at the Center for Wound Healing and Hyperbarics at Southwestern. “If you discover any kind of hot spot, even if it’s minor, it should be evaluated early to avoid life-threatening complications. Preventive care is extremely important when it comes to pressure injuries.”
Here are ten Pressure Injury Prevention Tips for Summer Vacations:
The Center for Wound Healing and Hyperbarics at Southwestern specializes in the healing of chronic wounds. Our team is specially trained in treating wounds that have resisted healing after weeks or months of traditional treatment. To learn more about our services, click here or to schedule an appointment, call 580-531-6441.

The Center for Wound Healing and Hyperbarics at Southwestern recently installed an additional hyperbaric oxygen chamber. The investment expands the community’s access to the beneficial outcomes oxygen therapy can provide to those with chronic or hard-to-heal wounds.
Oxygen is vital for the progression of wound healing by promoting cell proliferation, angiogenesis (the formation of new blood vessels), and protein synthesis – key processes in tissue regeneration. Any deficiency in oxygen during the healing stages heightens the risk of infection and delays recovery.
For patients who have low oxygen levels and have the appropriate indications, hyperbaric oxygen therapy (HBOT) can increase their oxygen levels up to 10 to 20 times more than normal. This is from breathing near 100% pure medical grade oxygen in a sealed chamber.
“HBOT offers patients a noninvasive treatment course using the power of oxygen and pressure to affect their overall healing.” explains Dr. Jennifer James “We are very excited to expand our HBOT services allow for greater access to those in our community who can benefit most.”
The Center for Wound Healing & Hyperbaric at Southwestern Medical Center uses advanced wound care modalities and hyperbaric oxygen therapy to treat non-healing wounds. Stalled wounds can be diagnosed, effectively managed and healed, oftentimes within eight weeks.
HBOT can be utilized for the following issues:
For more information about the benefits of HBOT or other services provided at The Center for Wound Healing and Hyperbarics at Southwestern, call 580-531-6441 or visit SWMConline.com/wound-care.
To explain why Wound Care is overwhelmingly essential to the lives of thousands of people, one must truly understand what exactly Wound Care is. Many people believe they know what it entitles; stitches, staples, wraps, and ointment. However, that is far from the reality of it. Wound Care is the complete management of a non-healing wound. Specialized wound care programs also play a vital role within the communities they serve. June is Wound Healing Awareness Month (WHAM), a time to recognize the challenges faced by individuals with non-healing wounds and increase awareness of how specialized care can save limbs and lives.
In the U.S, nearly 10.5 million people suffer from non-healing wounds, including diabetic foot ulcers, venous ulcers, and pressure injuries. Early evaluation and treatment are very important to help avoid complications including infection, sepsis, and even amputation.
One part of wound care is understanding the underlying comorbidities that patients have. The most common of these comorbidities is diabetes, which can greatly impact wound healing. Of the 34 million people in the U.S. who have been diagnosed, approximately 150,000 will lose a limb after a hard to heal wound becomes severely infected.
“In most cases, non-traumatic lower extremity amputations can be avoided,” said Catherine Yore, PA-C, wound care specialist at the Center for Wound Healing and Hyperbarics at Southwestern Medical Center. “With early detection, proper evaluation and specialized treatment, most wounds can be healed in eight weeks or less. Our primary goal is to help patients avoid the drastic measure of removing a limb, foot, or toe.” In fact, 74% of patients are able to avoid amputation in a wound center.
The Center for Wound and Hyperbarics at Southwestern Medical Center treats a variety of wounds and conditions, including radiation injuries to the tissues following cancer treatment. Treatment modalities include debridement, or the removal of dead skin and tissue to stimulate healing; and hyperbaric oxygen therapy, which can speed healing by carrying extra oxygen to the blood, organs and tissues. Our physicians may also recommend compression stockings, artificial skin, or negative pressure therapy.
Here are six things you need to know about specialized wound care:
If you or someone you love is suffering from a non-healing wound, contact our team of experts at the Center for Wound Healing and Hyperbarics by calling 580-531-6441 or click here for more information. We work with referring physicians to evaluate and treat non-healing wounds as quickly as possible, before they become life-threatening conditions.
Of the estimated 150,000 lower limb amputations performed in the U.S. each year, approximately 82 percent stem from a diabetic foot ulcer. When a patient with diabetes fails to keep blood glucose levels under control, a lack of blood flow to the lower limbs can result in the development of ulcerations or open sores. Symptoms include redness, increased warmth or firmness around the wound, swelling, extra drainage, pus or odor.
Some patients with diabetes can also develop peripheral neuropathy, or a loss of sensation in the lower limbs and feet. A simple cut or scrape can remain undetected and quickly develop into a severely infected wound. Patients often find themselves in the ER with a systemic infection and need urgent treatment.
It’s important for anyone with diabetes or cardiovascular disease to examine their feet and legs daily. If a wound does not heal on its own within 30 days, the risk of amputation and early death increases. In fact, a recent study shows that lower limb amputations have a three-year mortality risk of 71 percent.
“A chronic diabetic foot ulcer is one of the most common conditions we treat, and early evaluation is critical to help avoid limb loss,” said wound care specialist Catherine Yore, PA, Center for Wound Healing and Hyperbarics at Southwestern. “With proper intervention, most hard to healing wounds can be healed within four to six weeks and in most cases, amputation can be avoided.”
Wound treatment typically includes debridement, or the removal of dead tissue, management of the infection with the application of advanced wound care dressings or medications, off-loading or taking pressure off the area, and of course, keeping blood glucose levels under control. When a wound still does not respond to standard treatment, hyperbaric oxygen therapy or cellular tissue products (skin substitutes) may be indicated.
It’s important to be proactive and examine the feet and legs every day. Here are four tips for limb preservation, particularly for individuals with diabetes:
The Center for Wound Healing and Hyperbarics at Southwestern Medical Center consists of a multidisciplinary team of specialists dedicated to healing wounds, saving limbs, and improving the lives of our patients. For more information or to schedule an appointment, call 580-531-6441.
Peripheral Artery disease (PAD) is a common circulatory problem that affects over 8.5 million U.S. adults and it has a 5 times higher mortality rate than leading cancers. Stemming from fatty build-up, or atherosclerosis, in the arteries, PAD causes blood vessels in the limbs to narrow. This can significantly reduce blood flow which can lead to a non-healing wound if an injury occurs. If left untreated, these wounds can become infected, and put patients at risk of sepsis, gangrene, or even amputation.
Risk factors include aging, diabetes, obesity, and smoking. However, only around 25% of the population is aware of the disease, and many go undiagnosed. Symptoms include pain, cramping, discoloration, and swelling of the legs or feet. The most common wound types associated with PAD are Arterial, Venous, and Diabetic Foot Ulcers.
Tips to Manage PAD:
With lifestyle changes and a commitment to treatment, PAD can be managed. Here are eight tips to help:
At the Center for Wound Healing and Hyperbarics at Southwestern Medical Center, we’re using advanced wound care modalities and hyperbaric oxygen therapy to treat non-healing wounds caused by peripheral artery disease, including venous and arterial ulcers. Stalled wounds can be diagnosed, effectively managed and healed, oftentimes within eight weeks. If you or someone you love has a non-healing wound, give us a call at 580-531-6441 for more information and assistance or click here.
Come August with the sweltering temperature, it’s either in-door, in-water, or in-the-dark activities only to beat that late summer heat. However, whether you are scampering across the “cool” deck to the pool, or finally kicking back on the patio after the sun goes down, the heat is still there. And so is the risk of developing a wound. Especially for the 37.3 million Americans living with diabetes. Good thing Woundless Summer goes all summer long, because we’ve got all of the party favors to keep patients woundless during those hot Summer Nights, and what to look out for as summer comes to an end.
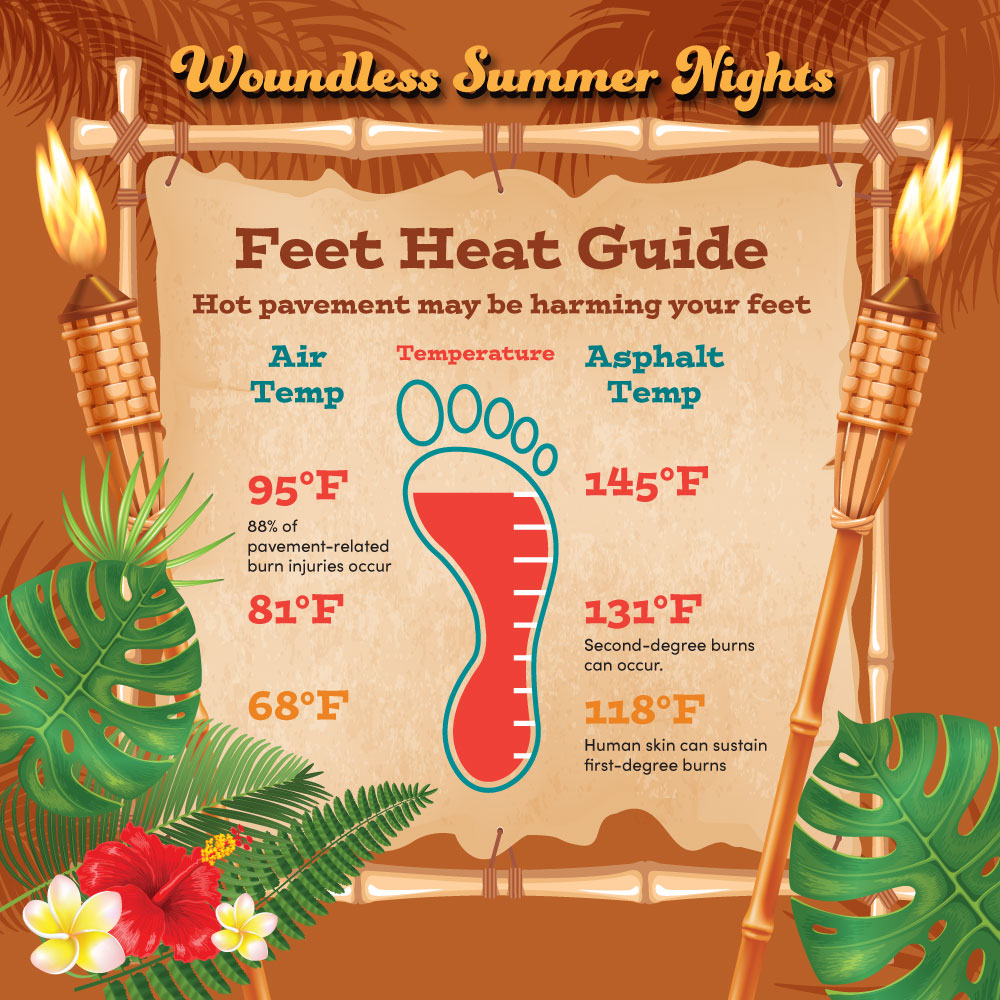 August can be brutally hot, and even when the sun goes down things like sand, pavement, concrete, and even that fancy cool-deck can still be holding the day’s trapped heat. So, before kicking off your party shoes after sunset, consider how hot it was that day. Anything that is above 111 degree Fahrenheit can start to damage the skin when touched, and at 118 degrees (just TWO degrees below the temp of a rare steak) the skin will experience a first-degree burn. And the only thing that should be burning hot on a Woundless Summer night is the grill.
August can be brutally hot, and even when the sun goes down things like sand, pavement, concrete, and even that fancy cool-deck can still be holding the day’s trapped heat. So, before kicking off your party shoes after sunset, consider how hot it was that day. Anything that is above 111 degree Fahrenheit can start to damage the skin when touched, and at 118 degrees (just TWO degrees below the temp of a rare steak) the skin will experience a first-degree burn. And the only thing that should be burning hot on a Woundless Summer night is the grill.
The heat is why the beach, poolside, or the patio, are the best places to celebrate during a warm summer night. All with the goal of waking up without a new wound the next morning. And a headache. However, those with Diabetes, especially those who are experiencing neuropathy, should always perform regular foot checks after a long summer night out, or can we be honest here and just say the entire summer? Between the heat, wearing sandals, and probably not drinking enough water between adult beverages, the feet are the best way to tell if it was truly a Woundless Summer.
Before whipping out the magnifying glass or hand-held mirror, here is what to look for on the foot:
Any one of these can lead to a Diabetic Foot Ulcer and should be monitored closely. If healing does not begin within the first two days, especially if the skin has broken, a doctor should be contacted immediately for further investigation. To prevent further skin damage, be sure to moisture the feet daily, especially if those dancing shoes did come off, or if time was spent barefoot in and out of a pool.
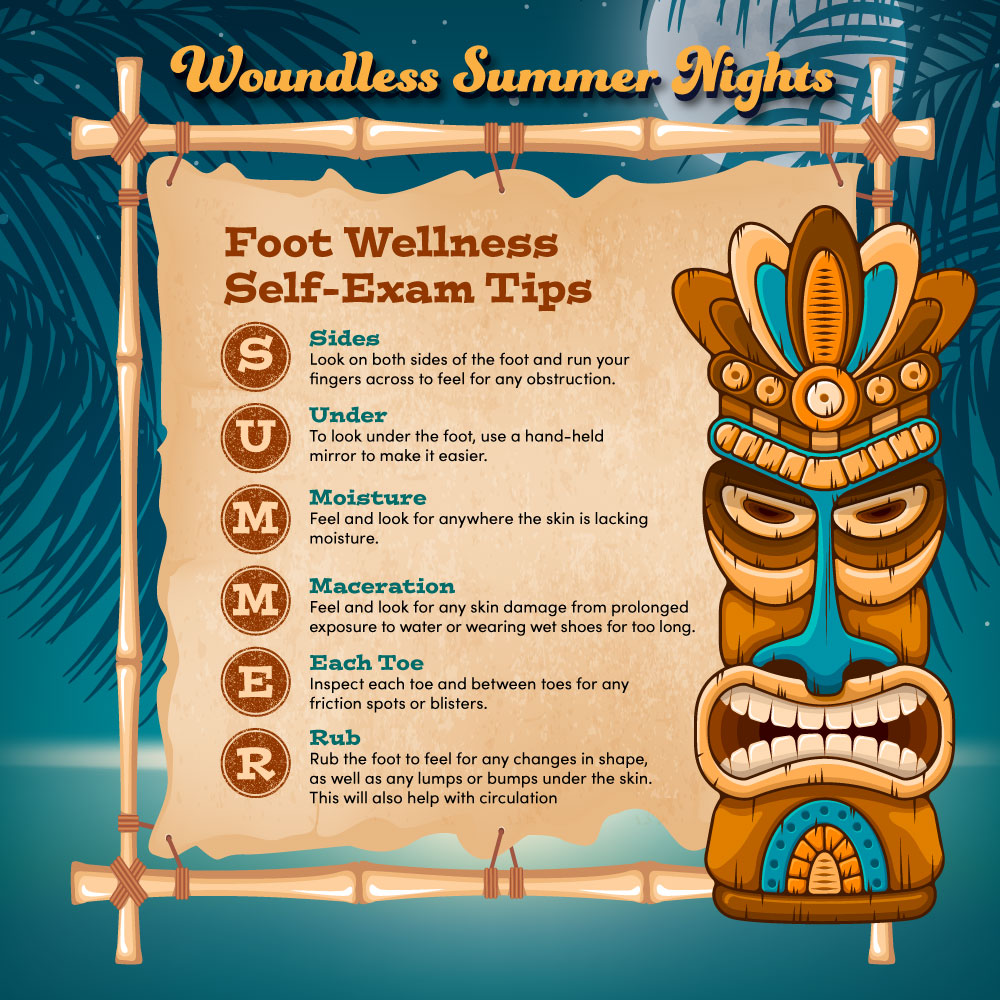 When it comes to the process of looking at the foot for any sign of a new wound developing, remember SUMMER:
When it comes to the process of looking at the foot for any sign of a new wound developing, remember SUMMER:
With SUMMER and CCR (not the band, but cuts, cracks, and redness), Woundless Summer can continue to live on, even long after the days become short, and the leaves begin to change. Light the tiki torches and cheers to the beach, summer camp, and the remaining warm nights ahead of us.
The Center for Wound Healing and Hyperbarics at Southwestern Medical Center is highlighting Wound Healing Awareness Month (WHAM) in June. WHAM is a time to recognize those who are paddling through the rough waters of the healing process trying to catch a break. So, to truly celebrate Wound Healing Awareness Month, The Center for Wound Healing offers those living with or at risk of developing a chronic wound prevention and care tips for a Woundless Summer.
Living with a chronic wound is not all beaches and margaritas, and for the 8.2 million Americans affected by a wound, that’s their reality when trying to feel those summer vibes. Not only is living with a non-healing wound painful, but it can quickly pull you into the undertow if not properly cared for. In fact, every 30 seconds a diabetic patient suffers an amputation, and those who go through limb loss have a 60% mortality rate within 5 years of amputation. That means more limbs are lost to diabetes than to a shark out surfing.
Don’t flounder just yet. WHAM is dropping in with all the essential tips to continue healing and prevent future wounds while doing all things summer. Here are 10 tips to keep your feet woundless all summer long:
By following these tips and being aware of the impact the hot months have on your flippers; pool parties, standing around a barbecue, soaking in the long days, some of the best parts of celebrating the summer months do not have to be a total wipe-out on the healing process. Those living with a chronic wound should still be a part of the summer staples and enjoy them. Wear appropriate shoes, drink more H2O than sugary or alcoholic beverages, and score more points in the healing process.
If you or someone you love is suffering from a non-healing wound, contact the team of experts at The Center for Wound Healing and Hyperbarics at Southwestern Medical Center. They work with referring physicians to evaluate and treat non-healing wounds as quickly as possible before they become life-threatening conditions.
The Center for Wound Healing & Hyperbarics at Southwestern Medical Center is recognizing American Heart Month by offering information and tips to educate patients about heart health and chronic wounds. Heart disease is the leading cause of death in Americans, and each year nearly 700,000 Americans are diagnosed with heart disease, which causes about 1 in 5 U.S. deaths, according to the Centers for Disease Control (CDC). Related complications like vascular insufficiency or peripheral artery disease can result in the development of non-healing wounds putting patients at risk of infection, sepsis, or lower limb amputation.
Due to an aging population as well as an increase in heart disease, diabetes and obesity, the need for specialized wound care continues to grow. Currently, there are approximately 9-12 million Americans suffering from chronic wounds or non-healing ulcers on the lower limbs or feet. Many patients postpone treatment with hope that their wound will heal on its own, only to seek treatment after it has become severely infected.
“It is not uncommon for cardiology patients to develop painful, non-healing wounds stemming from poor circulation to the lower extremities,” said Catherine Yore, PA-C, wound care expert at the Center. for Wound Healing & Hyperbarics “If left untreated, this can progress to a life-threatening condition. It’s important for anyone with a non-healing wound to talk to their doctor as early as possible and get an evaluation in order to avoid sepsis or amputation.”
Common Wound Types in Patients with Cardiovascular Disease
Without proper blood flow from the heart chronic wounds can develop and not only fail to heal, but they can grow in size and become infected. Here are the three most common non-healing wounds for patients with heart disease:
Tips for Better Heart Health
If you have heart disease or are in treatment for a non-healing wound, it’s important to pay attention to your cardiovascular health. A healthy heart stimulates the circulation of oxygen and nutrient-rich blood throughout the body, skin, and tissues and stimulates the body’s healing process. Here are six tips:
At the Center for Wound Healing & Hyperbarics, we’re using advanced wound care modalities and hyperbaric oxygen therapy to treat non-healing wounds caused by cardiovascular disease complications including venous and arterial ulcers. Chronic wounds can be diagnosed, effectively managed and ultimately healed, oftentimes within eight weeks. If you or someone you love has a non-healing wound, give us a call at 580-531-6441 or click here for more information and assistance.
Peripheral artery disease (PAD) is a common circulatory problem stemming from fatty build-up, or atherosclerosis, in the arteries. Also known as peripheral vascular disease (PVD), PAD causes blood vessels in the limbs to narrow, significantly reducing blood flow and sometimes causing the development of a wound that is slow to heal. If left untreated, these wounds can become infected and put patients at risk of sepsis, gangrene, or amputation.
PAD affects over 8.5 million U.S. adults and over 113 million people worldwide. Risk factors include aging, diabetes, obesity, and smoking. Symptoms include pain, cramping, discoloration, and swelling of the legs or feet. If you’ve been diagnosed with PAD and have a chronic wound that hasn’t healed within 30 days, it’s very important to have it evaluated and treated in order to save the limb and control the disease.
Types of Chronic Wounds in Patients with PAD/PVD
Here are the three of the most common non-healing wounds for patients with PAD/PVD:
Tips to Manage PAD
With lifestyle changes and a commitment to treatment, PAD can be managed. Here are eight tips to help:
At the Center for Wound Healing & Hyperbarics, we’re using advanced wound care modalities and hyperbaric oxygen therapy to treat non-healing wounds caused by peripheral artery disease, including venous and arterial ulcers. Chronic wounds can be diagnosed, effectively managed and healed, oftentimes within eight weeks. If you or someone you love has a non-healing wound, give us a call at 580-531-6441 for more information and assistance.
Osteomyelitis, or an infection of the bone, occurs when bacteria travels through the bloodstream or an open wound, to a weakened spot in the bone or marrow. It is a growing concern in modern healthcare, particularly with the rise in antibiotic resistance bacteria. Individuals with diabetes are at high risk of developing osteomyelitis because they are more susceptible to the development of chronic wounds, particularly on the feet or lower limbs. When coupled with diabetic neuropathy, a loss of sensation in the lower limbs, the condition can fester for months without the patient feeling any pain.
Osteomyelitis can develop any time a bone is vulnerable or exposed: after a puncture wound or trauma, near a surgical site, after joint replacement, or as a complication after amputation. Approximately one in 675 U.S. hospital admissions each year (50,000 cases annually) is due to osteomyelitis. Patients with diabetes, immunocompromised individuals, and patients on hemodialysis are at increased risk. Here are answers to six common questions about osteomyelitis:
If you or someone you know has a wound that is not healing or if osteomyelitis is suspected, a wound care and hyperbaric medicine specialist should be consulted as soon as possible. For more information, contact the Center for Wound Healing & Hyperbarics at Southwestern Medical Center at 580-531-6441.
Ahh. . . Summer. Long hot days enjoying too much sun, sand between the toes, and the delicious benefits of outdoor cooking. The laid back vibes in these months are not the easiest to create when trying to thwart off a wound from coming on. Actually, the patients most at risk of developing a chronic wound are dealing with a strong undertow of conditions, like diabetes, and that can be a real buzz kill when it comes to summer fun.
If you have any underlying condition, like diabetes, you need to be vigilant about foot care while participating in summer activities. Any hot-spots or areas of concern appear on your feet during the summer months, contact your care team immediately, preventative care is always the number one priority.
Luckily, the surf is still up for those patients, just with some extra precautions. Before paddling out to the horizon, use the below tips for a solid tow-in to a Woundless Summer;
For a Woundless Summer to never end, practice prevention and always be prepared for the day ahead.
The Center for Wound Healing & Hyperbarics specializes in the healing of chronic wounds. Our team is specially trained in treating wounds that have resisted healing after weeks or months of traditional treatment. For more information or to schedule an appointment, call 580-531-6441.
“Packing for the journey was important. Six pairs of trunks, two boxes of wax, some modern sounds, and in case of injury, one Band-Aid.” - Endless Summer (1965)
But maybe throw in an extra Band-Aid or two!
Click here for more health-related articles on wound care prevention and treatment.
For many, summer is the perfect time to run barefoot on the beach or in a grassy park. But if you’re one of the 34.2 million Americans living with diabetes, going barefoot is one of the worst things you can do for your health. Exposure to hot sand, pavement, rocks, trash and debris can result in trauma leading to non-healing wounds that put you at risk of infection, sepsis, or amputation.
Many complex wounds begin with a very small scrape or scratch. Some diabetics have peripheral neuropathy, or a loss of sensation in the lower extremities due to nerve damage. Because of this loss of feeling, a wound can remain unnoticed for quite some time and become infected, making the individual more vulnerable to delayed healing, progression of wounds, and even sepsis.
Here are seven summer foot care tips for patients with diabetes:
The Center for Wound Healing & Hyperbarics at Southwestern Medical Center specializes in the healing of chronic wounds. Our team is specially trained in treating wounds that have resisted healing after weeks or months of traditional treatment. For more information click here or to speak to someone about scheduling an appointment, call 580-531-6441.
May is Skin Cancer Awareness Month. Did you know that 1 in 5 Americans will develop skin cancer in their lifetime? If detected early, most basal or squamous cell cancers are highly treatable. But in some cases, a more invasive cancer like melanoma may require surgery and radiation therapy. Skin grafting, or the removal of skin from an unaffected area and using it to cover lost or damaged skin, is sometimes also needed for wound closure and healing.
The surgical application of skin grafts or flaps can increase the likelihood of infection so great care must be taken during recovery. Some surgical sites do not heal properly because radiation can dramatically reduce blood flow and much-needed oxygenation to the skin and tissues. If wound healing is significantly compromised, the patient’s physician – typically an oncologist, dermatologist or plastic surgeon – may recommend hyperbaric oxygen therapy (HBOT) to promote healing and preserve the skin. It is a safe, non-invasive treatment that targets and repairs damaged organs and tissues.
During HBOT the patient is placed in a hyperbaric chamber and breathes 100 percent oxygen under atmospheric pressure up to three times higher than normal. This boosts oxygen levels in the affected tissues, helps prevent infection, and promotes healing by encouraging the formation of new blood vessels.
In addition to faster healing, HBOT can reduce the need for additional surgical procedures. It can also help patients avoid further trauma and negative psychosocial effects due to aesthetics. Many skin cancer patients who require skin grafting report that HBOT has given them a new lease on life.
If you or someone you love has had aggressive treatment for skin cancer and suffers from a non-healing wound, ask your physician about hyperbaric oxygen therapy. For more information, please contact the Center for Wound Healing & Hyperbarics at 580-531-6441.
by Padmashree Velury, MD, Primary Care Physician
Did you know that – according to the Asthma and Allergy Foundation of America – more than 50 million Americans suffer from a type of allergy each year? That makes allergies the sixth leading cause of chronic illness in the U.S. And seasonal allergies account for a big percentage.
An allergen is something your immune system reacts to when that something touches or enters your body. There are food allergens, skin allergens and – during certain times of the year – seasonal allergens like the tree and grass pollination that occurs in spring and summer.
When these seasonal allergens make themselves known, they can cause a litany of potentially miserable symptoms in many of us, like:
Misery may love company but, while these symptoms are common, it doesn’t make them any easier to deal with. Fortunately, there are some steps you can take to help manage your seasonal allergies and ease your springtime suffering.
Be aware. Many allergy sufferers actually experience year-round symptoms that aren’t as prominent or noticeable in the “off-seasons.” To better control your suffering and minimize your symptoms, it’s important to know what exactly triggers your allergies. An allergist can help you identify what’s causing your attacks and work with you to develop a plan to minimize your symptoms.
Additionally, check daily weather reports for pollen and mold counts so you’re better prepared for heading outdoors or deciding to stay inside that day.
Take action. In addition to making an appointment with an allergist, there are other actions you can take to protect yourself. If the pollen or mold count is high, or you know you’re going to be outside for a long time, think about wearing a mask to protect your mouth and nose from allergen invaders. You may also consider taking an over-the-counter medication before you head out for the day. And don’t forget to take a shower. Changing clothes and jumping under the water after being outside can help reduce your exposure to seasonal allergens.
If you’re still not receiving relief from your allergy suffering, talk to your primary care provider, who can help you plan a different treatment approach, which may include an allergist and appropriate prescription medication to curb your symptoms.
If you need relief from seasonal allergy suffering, Southwestern Medical Center can help. To find a provider or schedule an appointment, call 888-796-2362 or visit our find-a-doctor tab here.
SIDEBAR: Is it allergies or COVID-19?
It’s a question on many lips during spring and fall, when seasonal allergies are at their highest: are my symptoms “just” allergies or do I have COVID-19? The two ailments unfortunately do have many similar symptoms, but there are some differences. For example, while COVID-19 often results in a fever, allergies do not. Similarly, COVID-19 can often come with muscle aches, while allergies would not. Still, there is enough symptom crossover that - if you are experiencing symptoms and are not sure (and especially if you think you may have been exposed) – the best way to know for sure is to test for COVID-19 with an at-home test or receive a COVID-19 PCR test at a place of care.
by Catherine Phipps, PA, Center for Wound Healing & Hyperbarics at Southwestern
Last year, half of the nearly 2 million people diagnosed with cancer in the U.S. underwent radiation therapy to destroy malignant cells. Thanks to new developments in radiation oncology, many patients end treatment and start a new life chapter. However, even though radiotherapy is very good at killing cancer cells, it can also impact nearby healthy cells. Some patients experience delayed radiation injury – painful and occasionally life-threatening side effects that present themselves months or even years later.
Approximately 30,000 of the 2 million U.S. cancer patients treated with radiotherapy last year will eventually report symptoms including significant pain, infection, bleeding, and physical discomfort. Radiation damage can occur just about anywhere on or within the body including the head and neck, chest wall, abdomen or pelvis. For example, patients who receive pelvic radiotherapy for urological cancers may experience significant abdominal pain, urinary frequency or urgency, and blood in the urine. Patients with head or neck cancer can suffer from osteoradionecrosis, a condition in which bone tissue weakens and deteriorates. It is an unusual but serious complication that can result in death of the bone and surrounding tissues and can lead to bone exposure through the skin. Again, these symptoms can appear years after treatment.
The likelihood of radiation damage depends on several factors including a patient’s sensitivity to radiotherapy, the type and dose of treatment, and the location of the cancer. Scarring, infection, and a lack of blood supply to treated areas can result in damage or death of surrounding tissues.
Radiation injury can greatly impact a patient’s quality of life; therefore, finding symptomatic relief is worthy of investigation. For some patients, hyperbaric oxygen therapy can eradicate long-term damage, allowing them to get back to their lives and/or successfully undergo additional reconstructive procedures such as breast or facial surgeries. With limited treatment options for radiation damage, hyperbaric oxygen therapy is a viable non-invasive treatment to consider.
Hyperbaric Oxygen Therapy: Providing Symptom Relief for Patients with Radiation Injury
First used in the U.S. in the early 20th century, hyperbaric oxygen therapy (HBOT) has emerged as a very effective treatment for patients suffering from the late effects of radiotherapy. HBOT can revitalize damaged tissues by bringing nutrients and oxygen to the areas that need it most through the growth of new blood vessels and increased circulation. This stimulates the healing process and can greatly improve the patient’s quality of life.
During treatment, the patient is given 100 percent oxygen in a pressurized hyperbaric chamber. The increased oxygen greatly enhances the ability of white blood cells to kill bacteria and reduce inflammation while allowing new blood vessels to form in affected areas. In other words, it speeds and promotes healing.
Hyperbaric oxygen therapy is very helpful for patients suffering from radiation injury because exposing the body to high levels of oxygen under pressure increases blood flow and vascularization to the area, which promotes healing. Increasing oxygen concentrations in the blood can be a tremendous help for people with radiation damage or chronic wounds. It offers a huge potential benefit with low risk.
How Do You Know if HBOT Treatment Might Help?
If you are a cancer survivor experiencing considerable pain or discomfort months or even years after radiation therapy, consult your physician. If HBOT is indicated, treatment should begin as soon as possible. Most insurance companies will cover HBOT with proper documentation. It should be noted that HBOT is a serious commitment of time and effort on the part of the patient, requiring daily appointments, sometimes for several weeks, for 10-60 treatment sessions. It’s important to note that HBOT is mostly reserved for outpatient treatment. For more information, contact the Center for Wound Healing & Hyperbarics at Southwestern, located at 5606 SW Lee Blvd. in Lawton, by calling 580-531-6441.

Southwestern Medical Center (SWMC) honored Bobby Gordon, the first Wound Care Hero Award recipient from the Center for Wound Healing & Hyperbarics, in a ceremony today at the hospital's Centennial Room.
In November 2020, Mr. Gordon contracted COVID-19 and was hospitalized and placed on a ventilator. His month-long battle to survive left him with painful pressure injuries (also known as bedsores) on several areas on his body. Upon discharge from the hospital, his physician referred him to the Center for Wound Healing & Hyperbarics for outpatient wound care.
“Serious pressure injuries require a significant commitment to treatment, on the part of the patient, to avoid infection, sepsis, and possible limb loss,” said Catherine Yore, PA-C and wound care expert. “Mr. Gordon’s wounds were quite severe and he has been seeing us every single week for almost a year. He’s been a model patient and his family has been very helpful with dressing and monitoring the wounds at home. He consistently enters our clinic with a cheerful greeting and positive attitude.”
Because of his extraordinary and inspirational commitment to healing, Mr. Gordon was honored with the Wound Care Hero Award. The award is sponsored by Wound Care Advantage and recipients are selected based on their commitment to treatment and positive attitude.
“I wouldn’t wish my experience with COVID-19 on anyone, and for a while I didn’t know if I was going to make it,” said Mr. Gordon. “I’m so appreciative to the wound care team at Southwestern Medical Center because they have been so respectful, caring and professional. They took really great care of me.”
“Our entire staff has enjoyed getting to know Mr. Gordon and his family and he’s almost ready for discharge,” said Yore. “We want his wounds to heal so he can be as close to his previous status as possible, but we’re also going to miss him when he ends treatment!”